Observations on Working with Over 100 People
I began my journey with bioenergetics close to two years ago under the guidance of Jay Feldman and Mike Fave. After having a few remarkable successes, I transitioned my clients into this paradigm and now have a data set of roughly 100 people, generally aged from 40-65yo approximately 60% women, 40% men. In my thirtieth article, I want to share my observations on successes and common pitfalls among clients while trying to distill key principles that you can use as guideposts.
TLDR:
Most people are under-eating calories and carbs but over eating fat (and the wrong kind)
Getting over the “sugar is bad” myth is difficult
Most people have micronutrient deficiencies, and usually the same ones
Most people aren’t sleeping well
Most people are out of touch with their body’s signals
Normal is not healthy (anymore)
It takes effort to be abnormally healthy
Most People are Under-Eating Calories and Carbs but Over Eating Fat (and the wrong kind)
I have noticed there is a sense of pride if someone feels they aren’t hungry for breakfast, can fast til noon, and eat one meal/day. This requires willpower and expresses a strong desire to improve health and I commend that. Just having the desire to maintain or get healthy is rare these days.
However, training yourself to be comfortable skipping breakfast or going OMAD means one has successfully lowered metabolic rate and overall energy production. The body is constantly vigilant to environmental signals, which include your total calories and carbohydrates, and will respond accordingly. Put the body into a state of scarcity and it will down regulate sex hormones, gut and muscle repair, wake you up at night, shorten your sleep, inhibit your mental recall, and cause brain fog.
The return to health requires systemic, tactical actions that essentially reverses the method one used to get themselves into poor metabolic health. This means creating a trajectory of eating as many calories as possible without gaining fat mass.
A big obstacle is that most people are time scarce so skipping meals is convenient. Between work, commuting, a family and trying to “have a life” the first thing that is sacrificed are three square meals. Additionally, when these individuals do fuel themselves (if they’re being health conscious), they’ll typically do it with animal products that have a lot of fat. Fat and protein are more satiating than carbs. Fat also has more calories per gram than carbs. So one feels the need to eat less.
If someone isn’t health conscious the food choices are from the most convenient (most processed) options. Snacks and packaged foods are generally high fat and no longer made from saturated fats but seed oils. They are typically more fat than carbs. The quintessential example is the donut - 55% fat from seed oil, 45% carbs.
Getting Over the “Sugar is Bad” Myth is Difficult
I understand why and was operating with this script for a long time too. It’s obvious, insulin resistance is bad. If you have insulin resistance and you simply add more sugar to your diet it will get worse. Insulin resistance is upstream of every metabolic disorder. Everyone agrees on this. However, sugar is not the cause of insulin resistance but rather the inability to metabolize sugar that causes insulin resistance.
One of those mitochondrial inhibitors is called the Randle Cycle and once I saw it employed in my body I let go of the fear of sugar. After running a 20% fat, 55% carb, 25% protein diet all my metabolic markers improved.
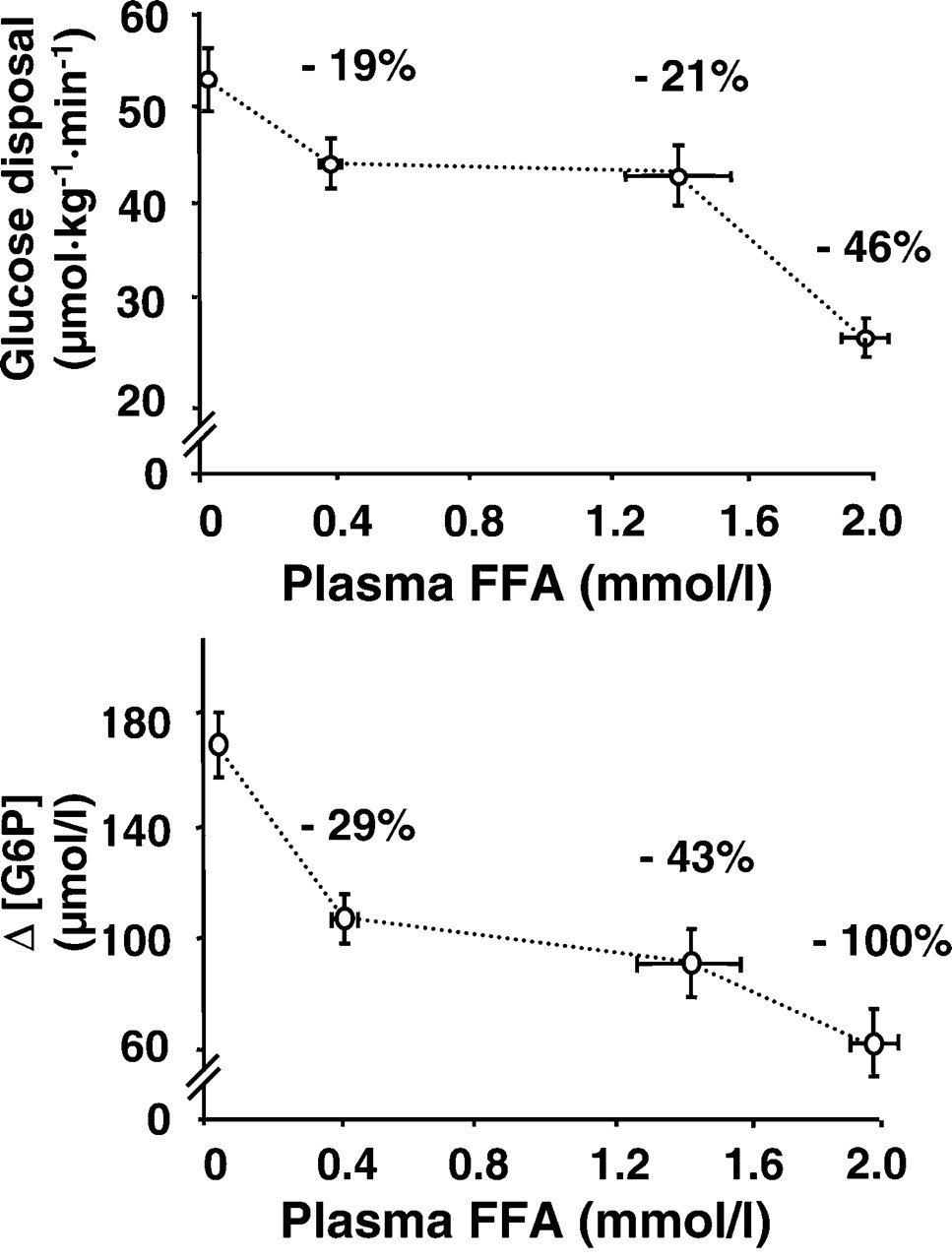
Simply put, the Randle Cycle is a metabolic switch that senses how much free fatty acids (FFA) are in your blood and when that amount reaches your personal threshold, the mitochondria will preferentially burn fat instead of sugar.
If this occurs because you are eating the same percentage of calories from fat and carbs (ie 40/40), FFAs will be high and the Randle Cycle will take effect. In this case what happens to the sugar you’re eating? It triggers higher and higher insulin levels to move sugar into storage (fat). This creates elevated fasting insulin, elevated triglycerides and over time, elevated fasting blood sugar and HA1C.
Another important thing to point out is that burning glucose increases the rate of energy production. A cornerstone principle in the low carb/keto space is that 1 molecule of fatty acid can produce more ATP than 1 molecule of glucose. This is true however the mitochondria don’t operate in a time vacuum. Per second, more ATP is produced with glucose compared to fatty acids. With glucose, the rate of energy production is higher, there’s lower oxidative stress, and more CO2.
Considering all of this, what do you think is a better solution to correcting insulin resistance - lowering fat or lowering sugar?
Most People have Micronutrient Deficiencies, and Usually the Same Ones
Sometimes micronutrient deficiencies are a cause of slower metabolic rate and sometimes they become the cause after metabolic rate is restored with a higher carb, lower fat diet. As metabolic rate increases, there is a greater need for vitamin and mineral cofactors. If they aren’t being supplied, you will experience a slow down.
Vitamin B1 and B3 are the two most common water soluble vitamins that are lacking for most people. B1 is critical for converting glucose into pyruvate and B3 is necessary to make and regenerate NAD. Both of these vitamins can create critical bottlenecks in glucose metabolism and should scale as you increase your carb intake.
Potassium, magnesium, selenium and copper are the most common mineral deficiencies I see. Correcting these either with foods or supplementation can dramatically improve energy production.
Potassium is the has the highest Adequate Intake (AI) recommendation of 4,700 mg/day for adults, making it the mineral with the highest daily requirement. This is more than double the AI for chloride (second highest), which is 2,300 mg/day. Its abundant in fruits, tubers (like potatoes) and squashes. If someone is low carb, they will definitely be deficient. Even if you’re not low-carb, you’re likely deficient.
Inland humans evolved in environments where dietary potassium was abundant (11,000–16,000 mg/day) and sodium was scarce (<700 mg/day), yielding a sodium-to-potassium (Na/K) ratio of ~1:16. Even coastal humans had higher K/Na ratios than modern diets. Today’s diets invert this ratio, with average intake at 3,400 mg sodium vs. 2,500 mg potassium (Na/K ≈1.36:1).
The other deficiency worth mentioning is selenium. Selenium is the rate limiting co-factor for T4 to T3 thyroid conversion. Moreover, in Hashimoto’s thyroiditis typically identified by elevated TgAb and TPOAb, the thyroid isn’t making enough glutathione with glutathione peroxidase enyzme (GPx) to balance the hydrogen peroxide created locally during the T4 construction process. If you’re deficient in selenium, you won’t make enough glutathione. Hashimoto’s patients have 40–50% lower selenium levels and GPx activity compared to healthy individuals.
Most of the time brazil nuts are recommended due to their high selenium content, however in bioenergetics we avoid them because their high PUFA content is antithyroid. Eating shrimp and oysters for selenium are the best food-based sources or simply supplementing has been shown to significantly reduce autoimmunity. Its worth noting that excessive iodine supplementation INCREASES Hashimoto’s hypothyroidism.
Most people aren’t sleeping well
If you have trouble sleeping defined by either the inability to fall asleep or stay asleep leading to shorter total sleep time you’re in a down spiral of what Hans Selye termed “Exhaustion”. Sleeping six hours is not as beneficial as sleeping eight. Sleeping from midnight to six is not as good as sleeping from ten to four. Not only does reduced sleep prevent regeneration, it causes further metabolic dysfunction.
This leads to another observation…
Most People are Out of Touch with Their Body’s Signals
Poor sleep is signal of negative energy balance. Why? The primary cause of inability to fall or stay asleep is elevated cortisol. Elevated cortisol is the body’s message that your stressors are outpacing your energy production. The metabolic consequences are increased lipolysis (FFAs) and gluconeogenesis (muscle breakdown). Elevated lipolysis and gluconeogenesis are pre-requisites for insulin resistance.
Under normal conditions, cortisol peaks in the morning to promote wakefulness and declines through the day, reaching its nadir at night to facilitate sleep. However, sleep deprivation or fragmented sleep disrupts this rhythm, leading to elevated evening cortisol levels. Partial or total sleep deprivation delays the cortisol quiescent period (the nightly drop), causing cortisol to remain elevated into the evening. Chronic short sleepers exhibit 45% higher cortisol levels compared to those with adequate sleep, perpetuating a state of hyper-arousal that inhibits restorative sleep.
This study found “When the integrated glucose and insulin responses were examined using the HOMA index, the area under the curve from 0900 to 1030 was >50% larger when the subjects were in the state of sleep debt than when they were fully rested.”
Sleeping from midnight to 6 AM (vs. 10 PM to 4 AM) delays the cortisol nadir, resulting in elevated daytime cortisol and impaired glucose tolerance. Night-shift workers, for example, exhibit 40% higher diabetes risk due to disrupted cortisol rhythms and insulin signaling.
Normal is Not Healthy (anymore)
Human health has been significantly downgraded over the last 4 generations. Body temperature is lower, people are eating less food, people are more micronutrient deficient, less fertile, sleeping worse, and we have more chronic disease because of metabolic derangement than ever before. All of this is despite the last 4 generations seeing more technological innovation in health care - pharmaceuticals, biomedical devices, diagnostics and surgical. It almost looks like they are inversely correlated.
This decline is also evidenced by lab ranges for blood work. Labcorp and Quest show us ranges for every marker. How are those ranges determined?
Labcorp’s reference ranges are derived from a database of over 45 billion test results, representing approximately 50% of the U.S. population. They use de-identified patient data to support clinical decision-making and population health efforts. Reference ranges reflect the middle 95% of results from the dataset, adjusted for demographics like age, sex, and geographic location.
Now consider that 60% of the U.S. population has at least one chronic disease, and 40% have two or more. This is the reference range used by our labs to denote “normal”.
It takes Effort to be Abnormally Healthy
By being healthy you are outlier. Your paradigm of health needs to be remarkably different if you want to be in the top 5%. To be abnormally healthy you need to recognize and take action on the fact there is a mountain of toxic burden in the food, water, air, clothing, skin care products, lighting, and nnEMF. Additionally the average person’s lifestyle operates orthogonal to nature’s rhythm. Your lifestyle and diet must be tailored around energy production and your stress tolerance threshold. It cannot reflect the 95%, it must different. If you don’t you’ll be outsourcing your biology to a system that has failed at chronic disease for the last 4 decades.
Your health is your legacy to your children and the future generations of humanity.
The Paradigm Shift
Make eating three square meals normal again
Waking up hungry is a gift. Being hungry for breakfast is being hungry for your day.
Take your meetings over a good meal
Start meal planning and team up with your partner to make it efficient
Revive the lunchbox and bring your meals with you
Tell your favorite restaurants you won’t eat there unless they use butter, coconut oil or tallow
Simple sugars in the form of fruit, honey, maple syrup, even brown sugar are the closest food to sunlight you can get
Align your circadian rhythm to the sun
To your health,
Jonathan
This is for informational purposes only and should not replace professional medical advice. Consult with your physician or other health care professional if you have any concerns or questions about your health.
Last week I wrote about the negative implications of COX-2 produced prostaglandins have on the upregulation of the aromatase enzyme. In the context of synovial health, we can see how detrimental it can be as well.
The entire category of pain medications known as non-steroidal anti-inflammatories (NSAIDS) specifically target the COX enzymes. These include aspirin, ibuprofen, and naproxen. Acetaminophen (Tylenol), not categorized as a NSAID, has weak COX inhibition. Avoid acetaminophen like the plague as it potently depletes your glutathione stores and can cause liver damage.
Of the three NSAIDS listed, aspirin was the first to be invented and is very safe. It has many beneficial properties of blocking COX-2 beyond dampening joint pain like improving glucose metabolism, protecting against seed oil conversion to PGE2 and inhibiting the aromatase enzyme.
Other natural COX-2 inhibitors include ginger (gingerol and shogaol), green tea (EGCG), and capers (quercetin).
Putting it all together
Optimize energy production using the bioenergetic diet and improving thyroid function.
Eliminate seed oils and replace with coconut oil, ghee/butter and tallow. Check all your packaged food and snack ingredients, you will be surprised how seed oils are everywhere.
Women, potentially supplementing progesterone.
Provide the raw material for producing collagen like bone broth, orange juice, beef liver, and oysters.
Consume COX-2 inhibitors like ginger, aspirin, green tea and capers.
Supplement Vitamin E (aromatase inhibitor).
To your health,
Jonathan
This is for informational purposes only and should not replace professional medical advice. Consult with your physician or other health care professional if you have any concerns or questions about your health.